What is Lymphedema?
Lymphedema is a condition of protein-rich fluid buildup that has the potential to occur wherever physical damage has been sustained in the body. Many of my clients have endured breast cancer treatments like radiation, lumpectomies, and mastectomies, which damage the vessels of the lymphatic system. Consequently, this protein-rich fluid – containing essential elements such as oxygen, protein, and white blood cells – becomes stagnant rather than freely flowing through the body.
This “dammed river” effect can result in a physical change- increased heaviness, limited movement, motion, and a “swollen appearance.” It can also produce strong emotional reactions due to the lack of a complete cure available and the understanding that this will always be a progressive condition.
There are two types of Lymphedema: primary and secondary. The congenital condition called lymphedema praecox, may have onset at birth or early on in a child’s life. It can also come when someone is in their 20s or 30s, during or after puberty (lymphedema tarda). Secondary Lymphedema is a condition that occurs after an event has affected your lymph vessels. For example, Filariasis is an infection from a nematode passed via mosquito bite. It disrupts the lymphatic vessels. The most common cause of Lymphedema in the United States is breast cancer-related lymphedema (BCRL).
The lymphatic vessel disruption is caused by surgery through surgical procedures such as lumpectomies and mastectomies, lymph node removal, and radiation treatment. Lymphedema can also occur due to chronic venous insufficiency in the lower limbs. Though lymphedema is often observed in the limbs, it can affect several parts of the body.
What is involved in the treatment of lymphedema congestion?
There are different stages of Lymphedema, and we use this staging system to help determine what types of intervention are needed at what frequency.
- Stage 0: Called the latent phase- may not see or feel any changes
- Stage 1: This is an early phase, symptoms of fullness/heaviness may come and go. Elevating the arm may reduce the size
- Stage 2: Symptoms always persist, often this is the phase when people seek and receive assistance
- Stage 3: The limb is considerably larger and is often referred to as “elephantiasis”
However, hope is not lost! A dedicated couple, Professor Michael Földi and Professor Etelka Földi, MD from Bavaria, Germany, studied Lymphedema extensively and devised a comprehensive protocol for healthcare providers assisting patients with similar conditions. They established a nutrition plan, an exercise program, and education on proper skin management and developed a unique massage therapy involving directional light touch and compression wraps performed twice daily.
This type of massage is called manual lymph drainage, and it uses anatomy to help “drain” the lymph fluid in the affected area. The entire process is called Complete Decongestive Therapy, or CDT. CDT consists of manual lymphatic drainage, exercise, skin care, and compression.
In Europe, the entire healthcare system is viewed differently. And to not get into the weeds of what design is better, let’s say they are very different. In Europe, people can go to this program for several weeks and stay there under a physician’s and physical therapist’s direct supervision. In the United States, we receive authorization for “X “number of visits.
So, in Europe, where you can get therapy sessions twice daily, some insurance companies limit you to twice weekly in the United States. Consequently, American therapists’ impact on their patients may be less transformative than their European counterparts.
It goes without saying that the impact of what therapists in the United States can do is less than what the therapists in Europe can do. It also limits those who are socioeconomically in a position where they cannot afford a cash-based therapy clinic that they can attend more often. This also affects clients living in states where access to health care, such as my own, may be limited. My state is relatively rural, and most of the population lives in a small area. This does translate to some clients having to travel one, two, or three hours to see a therapist with this specialty.
Despite these barriers, daily therapy with a knowledgeable professional is still ideal. At first, I held a bias against pneumatic compression devices as I viewed them as potential therapist replacements. However, my opinion evolved when I discovered that many patients had difficulty attending clinic appointments consistently.

The standard treatment of Lymphedema is divided into the intensive and maintenance phases. In the intensive phase, the client must have frequent intervention by a lymphatic therapist. In the maintenance phase, this can be done twice monthly to a monthly basis to achieve the best results. The effort of daily lymphatic drainage to reduce limb volume is on the client’s part.
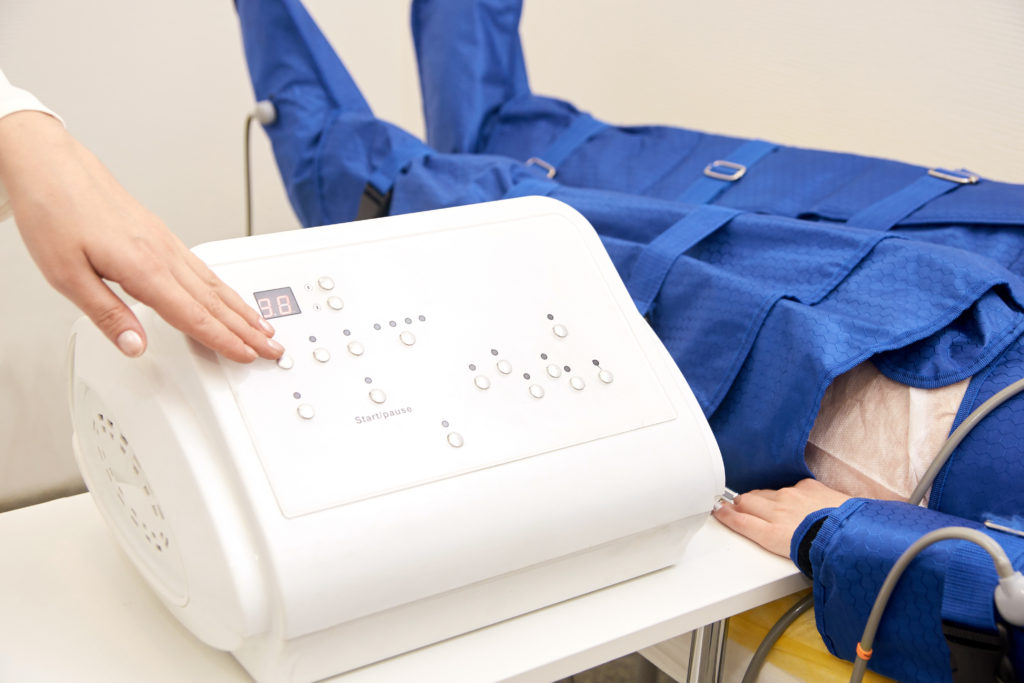
In concept, this is a great idea. However, it is considerably more challenging to complete manual lymph drainage on yourself, and to do this consistently on a daily basis is also tricky. A certain amount of consistent pressure is important to decongestive lymphatic therapy. This is where the use of intermittent pneumatic compression, a durable medical device (DME), in the home setting began to gain traction among clients and their providers.
Pneumatic compression therapy can treat patients with Lymphedema consistently and with ease thereby increasing a person’s quality of life. The use of compression can also lead to better results in the maintenance phase. A treatment plan of daily compression of the affected limb and trunk is more likely to keep Lymphedema in check.
The client first finds a position in which they are comfortable and in which the lymphatic fluid can move with less restriction. This is typically a reclined or full horizontal position. A Velcro compression sleeve is connected to a pump that intermittently inflates different sleeve segments.
How effective is a sequential intermittent pneumatic compression pump to treat Lymphedema?
Compression regimens are discussed between the lymphedema therapist and the client before discharge. Often, this will involve the use of the device twice daily, as the effects of increased lymphatic flow either through MLD or the compression device may last up to 5 hours.
At one time, I held a bias against pneumatic compression devices. I believed their purpose was for companies to bypass the need for a therapist and encourage people to work independently at home without the needed information to supplement treatment. There are genuine risks in thinking a machine can replace human interaction or provide targeted lymphedema treatment as effectively as an experienced therapist.
My perspective shifted as I realized that many individuals faced obstacles preventing them from visiting a clinic:
- Limited insurance authorization
- Denied insurance authorization
- Living more than 50 miles away from the clinic
- Balancing cancer treatments with clinic visits
- Limited financial resources
- Lack of physical stamina for clinic visits
- Full appointment schedules cause limited openings for clients
My view also changed when I saw a significant difference in the limb volume before and after the lymphedema compression pump had been used during the trial and a regular session. The relief that clients showed was tremendous.
So, seeing the reality of what many clients faced really started to take a toll, and I would say a positive influence on the way I looked at pneumatic compression devices. I requested them more often for my clients living further away or struggling to self-manage at home. When I say self-managed, it’s a person trying to mimic what a therapist does for a 50-to-55-minute session.
I have yet to meet anyone who can massage a certain part of their body for that long and not feel tired. Let alone reach all the areas they need for effective treatment. A comprehensive program that adds pneumatic compression as part of the maintenance phase may be the best option for individuals who are not physically capable of completing their own manual lymph drainage on a daily basis.
Next Steps
- If you aren’t actively being treated, seek out physical or occupational therapists certified in Lymphedema
- Certified lymphedema therapists have the CLT designation
- You can visit the Lymphology Association of North America to locate a therapy near you
- You can visit your healthcare provider and express interest in such a device.
Do insurance companies such as Medicare cover this?
This is the point of this article. The answer used to be long, confusing, and unclear to the health care providers. Mostly because of one phrase “the client must fail conservative treatment.” Matters grew more complicated when issues tied to the definition of “consecutive” therapy arose. What does failing conservative treatment even mean? Is it based on therapist-provided care or patients trying therapies themselves?
Interestingly, even the US Medicare system has supported this notion. In effect, pneumatic compression devices only receive payments once a client has “failed conservative treatment for four consecutive weeks.” This implies that assistance can only be accessed after hitting rock bottom. So, we have to ask ourselves: Is the failure of therapy really a success, or was the failure in the healthcare system as it was written?
In fact, what most people do not realize about their Medicare benefits, are terms such as Medicare local coverage determinations and national coverage determinations. My clients relayed to me that their primary concern when obtaining Medicare coverage was knowing whether they could afford the insurance payment from Social Security and/or retirement. They also expressed concern if their medications would be covered under Medicare Part D. We don’t tend to look under national coverage determinations to evaluate what we might and might not receive one day.
Sequential pneumatic compression pumps were designed to mimic what a lymphatic therapist does to significantly improve the limb’s volume. Why would this have to be shown to be ineffective? Why would a machine be able to produce results if regular treatment in the clinic was not? And what was the reasoning behind showing that the effectiveness of intermittent pneumatic compression would be superior to intermittent compression by the therapist?
A pneumatic compression device treatment session was to complete the management of Lymphedema at home and continue to have positive long-term effects long after the treatment was completed in the clinic.
But there are moments of hope – people who step up and fight back. Take the recent case of Greenwalt versus Becerra, where Mr. Greenwalt filed a civil action that challenged local coverage determinations for being unduly stringent compared to Medicare provisions on progressive compression devices. There is no longer a need to show that “4 weeks of conservative treatment” needed to fail to receive a pump for treating Lymphedema. I am a proponent of using healthcare research and quality to provide adequate treatment and controlled costs. However, the treatment that increases someone’s ability to follow a program which reduces the need for one-on-one treatment sessions also has value.
I am very excited about the changes for those who would benefit from pneumatic compression devices! Research has shown the efficacy of advanced pneumatic pumps for both Lymphedema and venous insufficiency management. It should be easier now for people to obtain the DME equipment they need.
In Good Health!
Bettina, Host of In the Rising Podcast
Interested in learning more about Lymphedema and scar tissue management? Learn more with this course:
Recovery to Function: A Guide to Rehab After Breast Cancer